The ongoing coronavirus pandemic is undeniably having widespread human, social and economic costs around the globe, and government and business leaders in every country are focussing their efforts to control its spread and impact.
From a pension scheme perspective, COVID-19 has had an adverse funding impact in most cases, with both asset values and scheme funding levels falling as well as employer covenants deteriorating, albeit to widely varying extents.
These asset-related funding issues may, however, be mitigated, to a limited extent, by the effect of the heavier mortality experience in curtailing future pension scheme liabilities. The scale of this will depend on the maturity of the individual scheme.
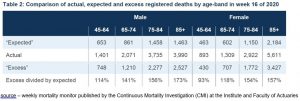
With some 90% of deaths occurring in the over-65 age group, more mature schemes are likely to experience a higher incidence of coronavirus-related deaths than schemes with a greater proportion of younger, non-pensioners. Also, since males have made up 60% of the COVID-19 deaths seen so far, schemes that have a greater proportion of males in their membership have had a heightened chance of premature deaths in recent weeks.
For smaller schemes, the population averages are less likely to be reflected, but some may see significant changes in their membership.
Of course, not all of these deaths are directly attributable to COVID-19. With huge social upheaval and operational changes in the healthcare sector, some individuals will find themselves at increased risk of non-coronavirus-related death due to changes in lifestyle or missing out on critical healthcare. This may be through choosing not to seek medical assistance (at least initially), or through having treatment cut back or delayed as resources are diverted towards treating those infected with the virus. The suspension of ongoing treatment for cancer patients in many parts of the country is one highly publicised example, although the much-feared scenario of an overwhelmed NHS being unable to treat seriously ill patients has thankfully so far been avoided.
The challenge in terms of predicting the longer-term implications for pension schemes is in understanding how all of this influences future expectations.
UK average deaths typically run at around 620,000 per year or c. 12,000 per week, albeit with seasonal differences. The number of COVID-19 related deaths witnessed to date should be seen in this wider context, with total UK weekly deaths presently running at around 22,000.
The CMI have put these UK recorded deaths into some kind of context for pension schemes by updating their standardised mortality rates on a weekly basis and comparing them with previous years. The chart below shows, unsurprisingly, that mortality experience over the past month is significantly higher than in the past. This contrasts sharply with the relatively benign results from 2019, which saw the lightest mortality for many years.
The full scale of the impact will ultimately depend on many factors including:
- how long the virus continues to take lives prematurely;
- to what extent these are balanced over time by a reduced number of deaths in the next few months or years;
- how quickly a vaccine can be found (and how effective it is);
- the extent to which the long-term health of those who have contracted the virus and survived has been affected;
- how quickly and effectively deferred treatment on other illnesses can be provided;
- the longer-term economic impacts in terms of household income/debt, which is typically correlated with life expectancy; and
- whether (and to what extent) there are knock-on effects from the lockdown in terms of causing other issues (the challenges to mental health are relatively well publicised).
Of course, there are potential upsides as well – the habits formed during lockdown may encourage people to exercise more regularly, spend more time preparing healthy meals, seek a better work-life balance and travel less. Again though, such aspects will be hard to measure and might vary widely across different segments of the population.
It is unrealistic to expect to have answers to all of these issues in the short term and the experience in other countries will not be entirely reliable as a guide, not least because of differences in testing infection rates, recording deaths, population density, age profile, underlying health levels, cultural behavioural norms, as well as in governmental and societal responses to the outbreak.
We should, therefore, avoid making any rushed judgments on the implications for longer-term rates, and be very mindful of the specifics of individual scheme populations. However, we should be confident it will be a source of much debate (and not just amongst pension actuaries) over the months and years ahead.